Eshealthtips.com – Posterior fossa brain tumors can be devastating. They often involve the brainstem. Cushing, who may have been the first to describe this condition, reported a high incidence of posterior fossa tumors in a large series. These patients had mostly fatal outcomes, but as an anesthetic and neurosurgical techniques have improved, the prognosis for patients with this condition is improving.
Patients with Posterior Fossa Lesions should Undergo MRI
Patients with posterior fossa lesions should undergo MRI to confirm the diagnosis. The MRI provides excellent anatomic and pathological details. The scan may also reveal abnormalities in structures surrounded by the tumor. Patients with suspected posterior fossa lesions should undergo a T1 or T2-weighted MRI.
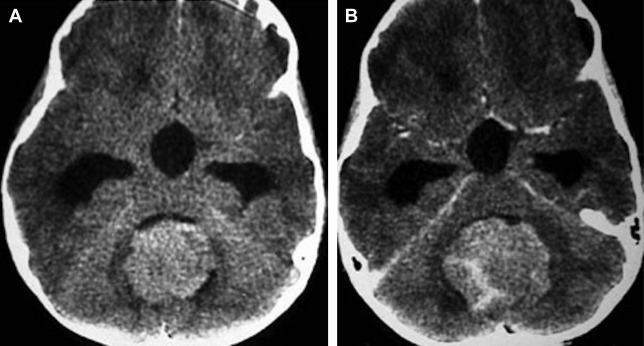
Children with posterior fossa brain tumors typically exhibit increased intracranial pressure, gait disturbance, and cranial nerve deficits. MRI and CT evaluation are essential for the work-up and management of these tumors. This article discusses the most common primary posterior fossa brain tumors and how they can be diagnosed and treated. If you or a loved one has a posterior fossa brain tumor, consult your family doctor or a neuroradiologist for help.

Although posterior fossa brain tumors are a challenging case for neurosurgeons, patient survival has increased significantly in the last twenty years. Recent MRI techniques, such as diffusion-weighted imaging (DWI), MR spectroscopy (MRS), and DWI, can help in improving diagnosis.
Posterior Fossa ADC Value Associated with Lesion Severity
These studies show that the ADC values of the posterior fossa are related to the severity of the lesions. Moreover, the ADC values are associated with the size of the lesions. To compute the mean ADC value, the largest posterior fossa lesion was selected.
Most posterior parts of the skull are lined with the brain. The posterior fossa is divided into three main locations. The right one houses the brain stem. The posterior fossa is bounded by the occipital bone and the squamous and mastoid temporal bones. It is the most posterior part of the skull. Various structures in the back of the head are located in this region. Besides, these tumors may press on delicate structures.
Researchers studied the morphology of the brainstem and cerebellum within the posterior fossa. The posterior fossa also contains the midbrain, pons, and medulla oblongata. They compared the volume of these regions of the brain in relation to the volume of the posterior fossa of the cranium. Using this method, they estimated the degree of overcrowding in the posterior fossa.
Early Diagnosis Can Help Prevent Complications
Posterior fossa brain malformations include hemangiomas, arterial anomalies, coarctation of the aorta, and eye abnormalities. However, there is no definitive diagnosis, although the condition is sometimes linked to arterial ischemic stroke. Despite the high prevalence of these conditions, the relationship between these conditions and AIS is still unknown.
The causes of this disorder are unclear, but an early diagnosis can help prevent complications and reduce hospital stays. Early recognition can also enhance patient and family understanding of the condition. This syndrome affects children and young adults. A comprehensive evaluation by a pediatric neuroradiologist can help in the management of patients.

MR spectroscopy provides an additional way to differentiate between benign and malignant brain lesions. The technique uses MR spectroscopy to assess the distribution of metabolites in the brain and help in diagnosis. The technique helps in evaluating the lesion’s size and location.
Reference: