Eshealthtips.com – In a 32-year-old Asian woman, acute stroke and recurrent right-sided transient ischemic attacks presented with no history of bleeding are suspected. She is diagnosed with stroke after a clinical workup is normal. She underwent a digital subtraction angiogram, which revealed an abnormal corkscrew-like appearance of the intracranial distal vessels. She was discharged with a single antiplatelet drug and has had no further transient ischemic attacks.
Intracranial Arteries Similar To Extracranial Arteries
Intracranial arteries are similar to extracranial arteries except that they do not have the vasa vasorum. They are also smaller and do not contain external elastic lamina. Larger intracranial arteries share many structural features with extracranial arteries. For example, they are not lined with cartilage, and their lumen is narrower. But their lengths differ. In addition, intracranial arteries lack valves and have a higher blood-brain-matter content than extracranial arteries.
Pial arteries are intracranial vessels that lie near the surface of the brain. They receive perivascular innervation from the peripheral nervous system. Parenchymal arterioles, on the other hand, receive intrinsic innervation from the brain’s neuropil. Luminal caliber and the number of collaterals are crucial factors in collateral supply. Venous collaterals serve as supplemental arteries to augment cerebral blood flow when primary routes are blocked.
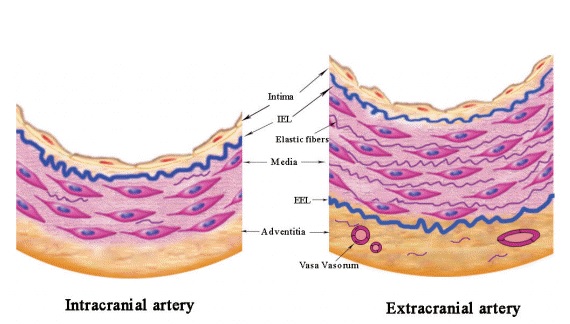
The IEL of intracranial arteries is thicker than that of extracranial vessels and has a characteristic fenestration pattern. It also lacks an external elastic lamina. Its adventitia is thick and contains few elastic fibers, and its thin walls may allow oxygenated blood to diffuse from the CSF. Thus, CDI may be used during a standard B-mode sonographic examination to identify the flow pattern.
Evaluating the Distribution of Blood Flow in the Brain
To evaluate the blood flow distribution in the brain, PCMRI techniques have been used. This technique is inexpensive, convenient, and easy to apply at the bedside. It may be useful in assessing the pathophysiology of cerebral ischemia. Moreover, the MCA may be the most relevant vessel for TCD imaging. A small overlap in the data helix and a slightly-overlapping pitch of the image improve the contrast-to-noise ratio.
Healthy cerebral arteries contain three concentric layers: a single layer of endothelial cells; a thick inner elastic lamina; and a single layer of smooth muscle cells. The middle layer is made up of collagen fibers, fibroblasts, and perivascular nerves. In addition, the walls contain pericytes and astrocytic end-foot. The IEL of intracranial arteries is highly developed.
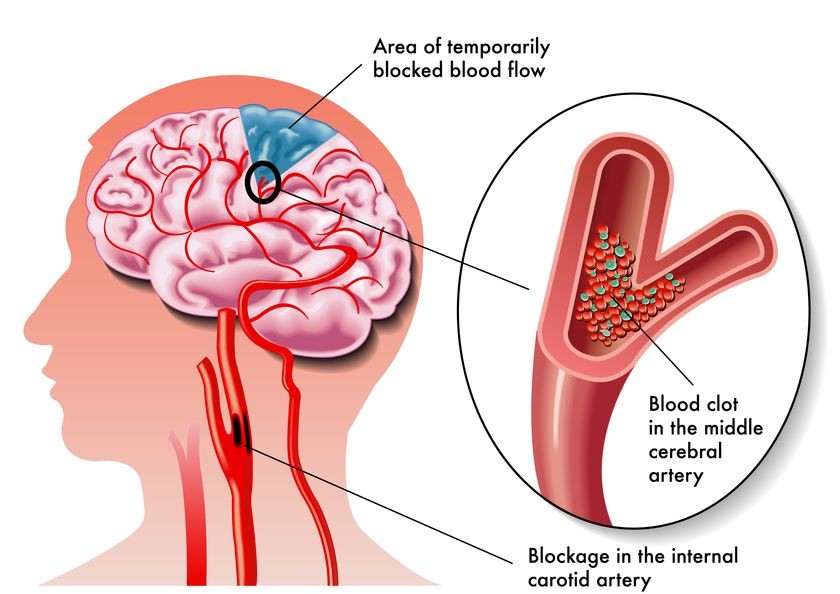
Circulation in the brain is critically important. Brain tissues use the greatest percentage of cardiac output and are highly sensitive to changes in nutrient supply. Abnormal flow to the neurocranium is a major cause of cerebrovascular disease, and several cerebrovascular disorders are closely related to abnormal flow in the brain. Acute disruption of blood flow in the brain can lead to stroke or ruptured plaques. Inflammatory flow may increase the risk of platelet aggregation.
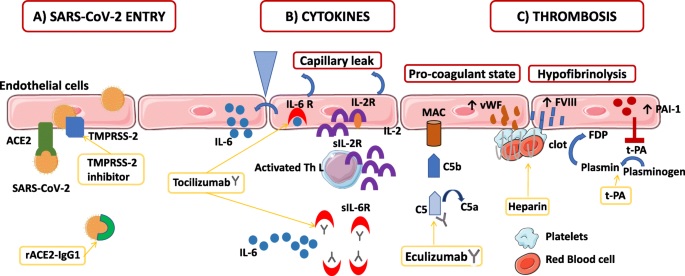
Causes Damaging Effects on the Endothelium
A study of spatiotemporal flow in the brain may provide useful clues to diagnosing and managing cerebrovascular disease. For example, biomechanical measurements of the velocity field adjacent to vessel walls may provide information about the presence of aneurysms or plaques. Alterations in vascular wall shear stress lead to deleterious effects on the endothelium and increase the risk of aneurysm rupture. It may also identify slow-flowing zones that are prone to embolisms.
The venous system of the brain is an interconnected network of veins. Venous outflow from the cerebral hemispheres occurs through the cortical veins and deep central veins. These veins empty into the inferior sagittal sinus and the great vein of Galen. Cerebellar drainage is accomplished through the inferior cerebellar vein and the occipital sinuses.
Moreover, cross-sectional research of patients was conducted to compare the effects of atherosclerosis on cerebral artery calcification. In patients with vascular disease, the calcified lesion on CT represents only part of the entire atherosclerotic plaque. Its “soft” part is presumed to be more vulnerable to damage since it does not contain calcium. Autopsy studies have found a relationship between cerebral artery calcification and the severity of atherosclerosis. Hence, intracranial arterial calcification may be associated with atherosclerotic changes in the distal cerebral vessels.
Reference: