Eshealthtips.com – Various factors play a role in the development of coccoid bacteria. They include infection, immune system, and biofilm formation. They also induce chronic inflammatory processes, invasion of mammary tissues, and resistance to antibiotics.
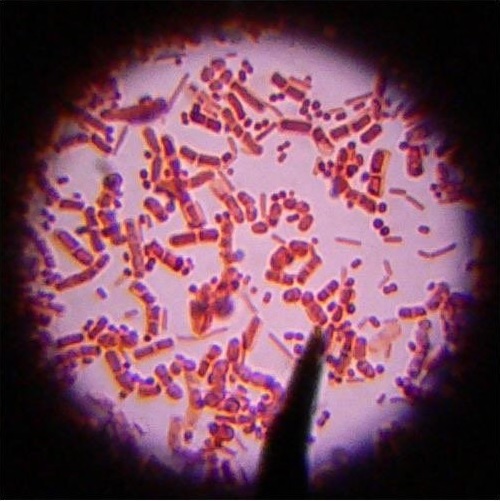
UPEC Produced Morphology of Coccoid Bacteria
During an acute urinary tract infection (UTI) in a mouse, uropathogenic Escherichia coli (UPEC) produces a coccoid morphology of bacteria. This morphology allows the bacteria to colonize naive uroepithelial cells and evade the host immune system. It also allows UPEC to survive urination and inflammation. These intracellular bacterial communities (IBCs) are biofilm-like and provide a protective environment for UPEC members.
These UPEC bacteria are found in both uncomplicated and complicated urinary tract infections. However, the morphology of UPEC is not uniform among isolates. Some UPEC isolates exhibit a filamentous morphology, which allows the bacteria to circumvent the host immune system. The filamentous morphology also makes UPEC resistant to neutrophil killing. Various types of microbes invade the mammary tissues of mice. These organisms colonize specialized alveolar epithelial cells. These organisms form intracellular microcolonies and induce a rapid inflammatory response, similar to LPS. Infected mammary alveolar epithelial cells exhibit pronounced cellular swelling and melanocytosis.
The invasion of mammary alveolar epithelial tissues by pathogenic bacteria is well-described in clinical cases of coliform mastitis in dairy animals. However, this pathology is very heterogeneous. The underlying mechanisms remain unknown. The pathogenic bacteria that invade mammary tissues are able to invade through various niches, including the mammary gland cistern, the stratified epithelia lining teat canals, and the duct spaces. This invasion might have occurred due to the activation of TLR signalling. In addition to TLRs, other bacterial molecules may also induce signalling.
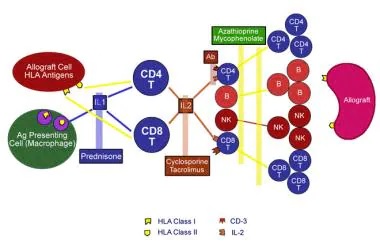
Factors Contributing to the Development of Immunosuppression
Various factors contribute to the development of immunosuppression in patients. The immune system is a complex system of defense that responds to pathogens through the production of cytokines. These cytokines interact with bacterial proteins, which may inhibit the activity of the bacteria. Infections, stress, and immunosuppression have been known to induce a reduction in the body’s immune response. This can result in increased mortality and increased susceptibility to disease. Several studies have shown that N-acetylcysteine (NAC) has antioxidant properties, which may protect cells from oxidative damage. It is also known to have antibacterial and anti-inflammatory properties. It inhibits the growth of gram-positive and gram-negative bacteria. Similarly, NAC inhibits the invasion of uropathogenic E. faecalis.
Biological biofilms are produced by bacteria that form a complex assembly of polysaccharides. These biofilms are found in the environment and in human bodies. The composition of the biofilm matrix varies by species. It may contain glycopeptides, proteins, lipopolysaccharides, and nucleic acid. Some proteins associated with the biofilm matrix exhibit enzymatic properties, while others exhibit adhesive properties. Biofilms can form on a variety of surfaces, such as rocks, soil, and pipes. They can also develop on medical devices. A recent study identified biofilms in 62% of chronic laryngitis patients. This suggests that biofilms are a potential reservoir for infections in the future.
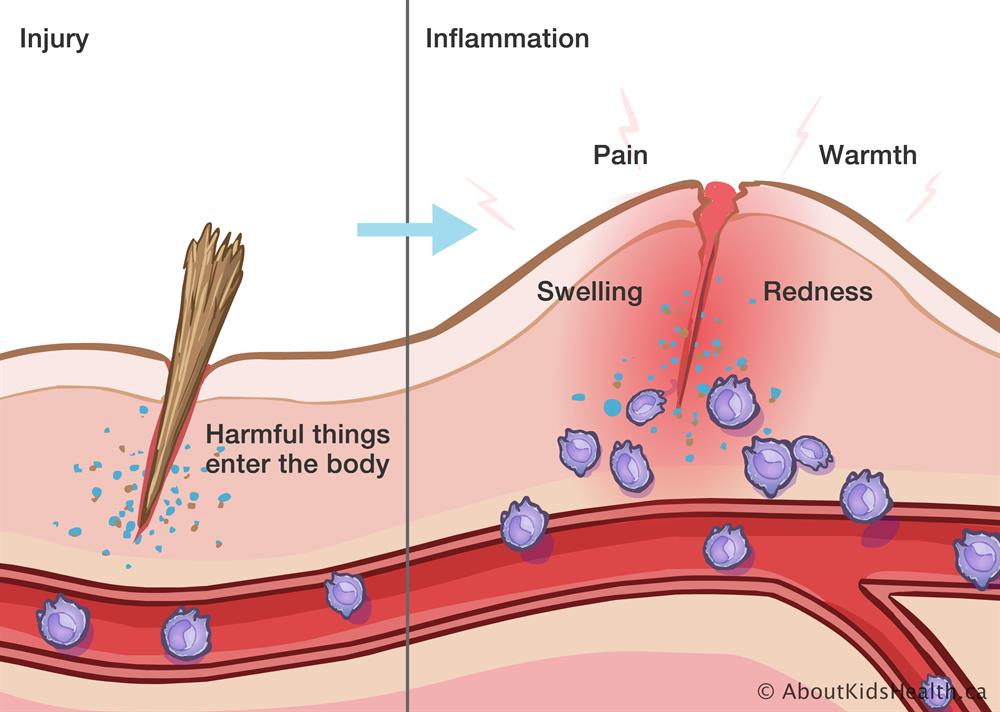
Biofilm formation is controlled by bacterial surface molecules, such as eDNA, flagella, and adhesins. These molecules are involved in surface-associated infection and contribute to the adhesive properties of the biofilm matrix. They also influence the architecture of the biofilm. Normally, inflammation is an innate immunity mechanism that is activated by harmful stimuli such as pathogens or foreign bodies. However, too much inflammation can lead to a bacterial infection or cause tissue damage. Inflammation is also associated with pain.
The First Stage of the Immune Response Against Pathogens
There are two types of inflammation: acute and chronic. Acute inflammation is a rapid response that is characterized by the movement of plasma fluid into inflamed tissues. It is a vascular response, resulting in marked vascular changes and redness. It can lead to tissue damage, but can also minimize the risk of infection. Acute inflammation is the first stage of the immune response to pathogens or other injurious stimuli.
Several types of bacteria have evolved sophisticated mechanisms of resistance to antibiotics. These mechanisms can be used to limit uptake, inactivate, or modify a drug. These mechanisms have increased the number of infections and added to the global impact of infectious diseases. Understanding the biochemical basis of resistance is important for designing therapeutic strategies.
Bacteria have remarkable genetic plasticity. They can acquire genetic material from related organisms, from abiotic sources, or through recombination. Bacteria can also acquire resistance genes from chromosomal DNA or through conjugation. These methods are most commonly used for transmission of resistance genes. Intrinsic resistance occurs when a subset of bacterial cells develops mutations in genes coding for the target site of an antibiotic. These mutations may be deleterious to the cell, but they often preserve the cells’ survival. Some of these mutations occur in drug transporters and regulatory networks. Other mutations can occur in genes encoding a drug’s binding site.
Reference: