Eshealthtips.com – In this article, we will explore the treatment of Thoracic Burst Fracture. While it is possible to safely perform this procedure with minimal radiation exposure, the international spine surgery community remains divided on its surgical guidelines. In general, the TLICS classification system is based on three major categories. The sum of these three scores indicates the severity of the injury. A TLICS score of 3 suggests nonsurgical treatment, whereas a TLICS score of 5 requires surgical intervention.
Treatment for Thoracolumbar Burst Fractures
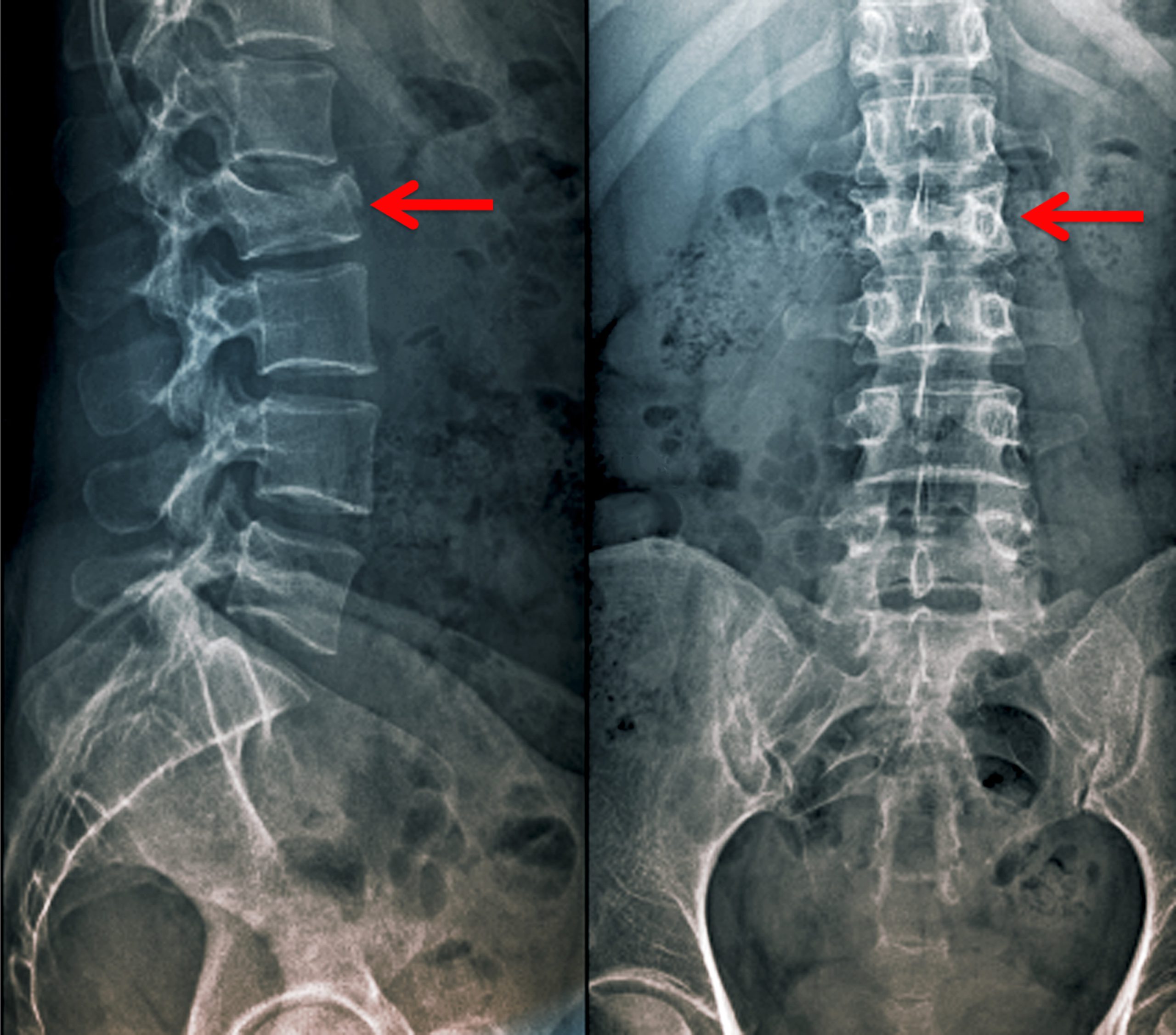
One recent study evaluated the use of TLICS to determine the treatment for thoracolumbar burst fracture. They analyzed data from 182 patients who underwent conservative treatment and surgery for thoracolumbar burst fracture. TLICS scored two or more in 21 patients with a stable burst fracture. Only 14 patients (66.7%) underwent an anterior or posterior fusion, while the rest underwent conservative treatment, including bracing. Three patients underwent percutaneous vertebroplasty.
The risk of an unstable burst fracture increases with the severity of the vertebral body compression. In these patients, operative treatment was necessary to prevent focal and progressive kyphosis. The pedicle screw operation has been approved for this purpose by the Korean Health Insurance Review & Assessment Service Center (KHRAS).
Significant between Treated with Buffer and Not
Although Bailey et al40 found a significant difference between patients treated with a brace and those with no treatment, the study’s results were not blinded. The SF-36 score and RMDQ scores were unaffected. It did not use a standardized diagnostic method and did not include patients with compression fractures or unstable thoracic fractures. However, the researchers did provide level II evidence.
While the specific causes and management of thoracolumbar burst fractures are unknown, there are a few important factors that can affect the outcome. One of these factors is the existence of traumatic spinal canal stenosis. It also influences the fracture’s severity and the type of surgery required. The patient will be at risk for neurological deficits as a result of the fracture. The best way to manage a thoracolumbar burst fracture is to undergo surgical treatment.
Nonoperative Treatment of Thoracic Burst Fracture
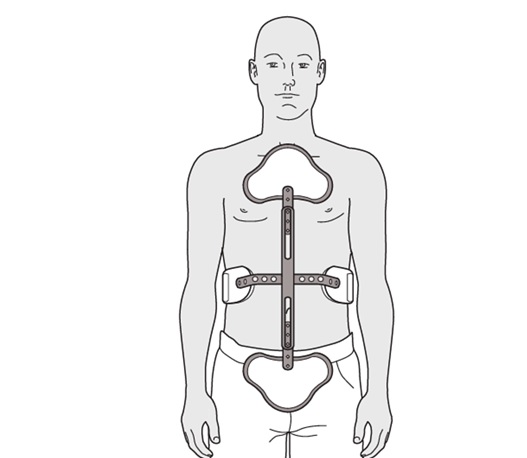
Nonoperative treatment of Thoracic Burst Fracture has no standardized guidelines. Evidence from randomized controlled trials shows that external bracing improves pain relief in patients with neurologically intact injuries, while minimally invasive surgery has no proven benefit. Furthermore, nonoperative treatment without a brace can optimize resource use, engage patients, and provide additional viable options. Therefore, this guideline aims to answer the question of whether external bracing is beneficial for patients with this condition.
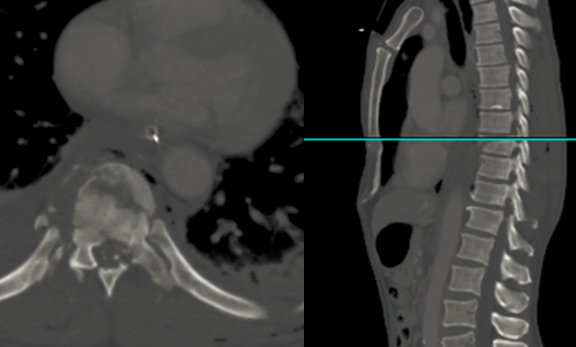
This study presents a case of subacute T11 burst fracture, resulting in severe cord compression and posterior bony retropulsion. Complications of this fracture include segmental kyphotic deformity, urinary retention, and patchy sensory loss. The patient’s MRI showed a seventy percent loss in vertebral body height and an 8-mm posterior bony retropulsion of the bone into the spinal canal. The cord also showed a T2-weighted hyperintensity, which is indicative of cord edema.